BACKGROUNDPosterior reversible encephalopathy syndrome (PRES) is a variable cerebrovascular syndrome related to hypertension and autoregulatory failure. Steroids have been reported to each precipitate and deal with PRES.
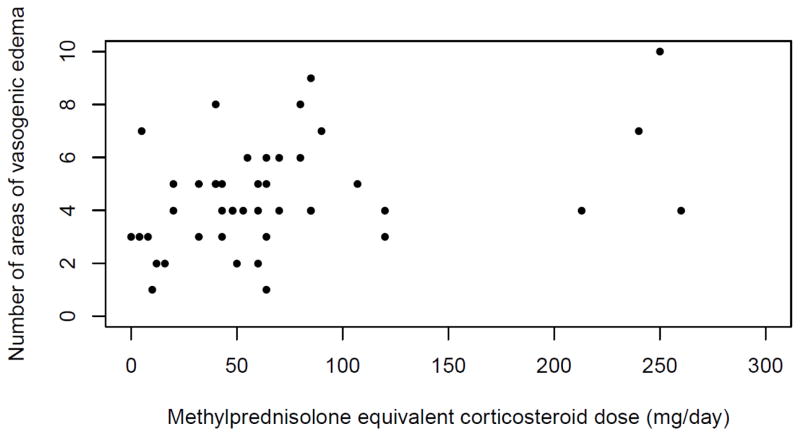
We sought to find out the prevalence of steroid therapy on the time of PRES and to evaluate the connection between steroid therapy and extent of vasogenic edema.
METHODSWe carried out a retrospective evaluate of radiology stories between 2008 and 2014 from two educational medical facilities to determine instances of PRES. Clinical and radiographic knowledge have been collected.
Descriptive statistics have been used to find out the prevalence of corticosteroid therapy on the time of PRES onset and the latency from steroid initiation to PRES onset. The affiliation between steroid therapy and extent of vasogenic edema was assessed in a number of regression fashions.RESULTSWe recognized 99 instances of PRES in 96 sufferers. The median age was 55years (IQR 30-65) and 74% have been ladies.
Steroid therapy at time of PRES onset was recognized in 44 of 99 instances. Excluding sufferers on power therapy, the median length of steroid publicity earlier than PRES onset was 6 (IQR, 3-10) days.
Steroid therapy was not related to extent of vasogenic edema in unadjusted or linear and logistic regression fashions adjusted for age, intercourse, and most systolic blood stress on day of onset.CONCLUSIONSCorticosteroid therapy, usually of temporary length, often preceded the onset of PRES and was not related to severity of vasogenic edema.
The position of bradykinin in the etiology of vasogenic mind edema and perilesional mind dysfunction.
The feline infusion mannequin of mind edema was used to guage the position of bradykinin in the etiology and pathophysiology of vasogenic mind edema. Bradykinin (Three or 90 ug in 600 microL saline) didn’t alter normocapnic regional cerebral blood movement (rCBF) nor induce particular modifications in both the somatosensory (SEP) or motor (MEP) evoked potentials.
The imply will increase in ICP (from 4.5 to 16.1 mmHg) and peri-infusion white matter water content material (from 69.Four to 79.eight ml/100 g tissue), imply lower in lumped craniospinal compliance (from 0.040 to 0.014 ml/mmHg) and native histological modifications have been all just like these after 600 microL saline infusion.
The interstitial bradykinin infusion induced focal blood-brain-barrier (BBB) opening to Evans Blue dye and was chemotaxic for granulocytes. After the infusion there was a worldwide loss of rCBF CO2 reactivity however there was no ischemia at normocapnia.
These outcomes present that bradykinin in mind edema fluid, at concentrations higher than these discovered in neuropathological circumstances, can open the BBB of regular cerebral parenchymal capillaries and trigger vascular dysregulation.
In neuropathological circumstances bradykinin could due to this fact potentiate formation of vasogenic mind edema however doesn’t contribute to perilesional mind dysfunction.